Abstract
Introduction: Autologous stem-cell transplantation (ASCT) is considered as the standard of care for transplant-eligible multiple myeloma patients (TEMM), but no randomized trials have assessed the optimal number of induction cycles or the ideal depth of response required before ASCT. Whether it can lead to the presence of tumor cells in stem cell collection (SCC) without complete response (CR) before ASCT and impose negative impact on survival is being debated. Here we evaluated the effect of the minimal residual disease (MRD) of SCC on TEMM.
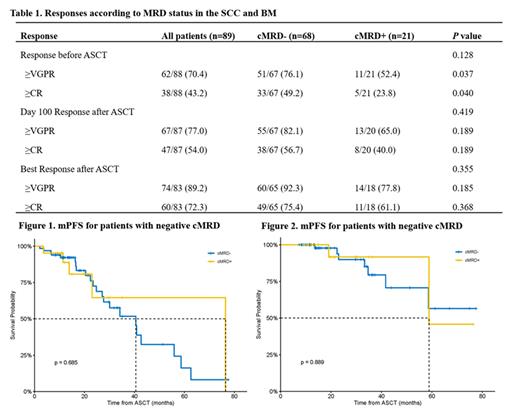
Methods: We analyzed clinical data of 89 MM patients undergoing ASCT between January 1, 2013 to June 1, 2021 in our hospital. MRD evaluation of both BM (mMRD)and SCC (cMRD)were carried out at the same time before ASCT. Response assessment was defined according to International Myeloma Working Group criteria. MRD was evaluated by multiparameter flow cytometry (MFC) with 10-5 sensitivity. Time from ASCT to disease progression was defined as modified progression-free survival (mPFS) and time from ASCT to death as modified overall survival (mOS).
Results: A total of 89 patients met the inclusion criteria. The median age is 54 (37-69) and 62.9% were males. There were 24 (27.0%) patients presenting high-risk cytogenetic abnormalities by FISH, defined as the presence of at least one of t (4;14), t (14;16) or del (17p). Before ASCT 31.5% of patients achieved MRD negativity in BM and 76.4% in SCC. By comparing the MRD-positivity status with different sensitivity and numeric levels of tumor cells, we found the percentage of patients with MRD-positivity in SCC was much less than that in BM (P <0.001). Residual tumor cells were observed in the SCC in approximately 20.5% and 25.0% of patients who had attained CR/sCR or VGPR after induction therapy, respectively. Although a higher percentage (38.5%) of cMRD positivity was observed in patients with PR before ASCT, but there were no significant differences among the three subgroups (P=0.126). Approximately 29.8% (26/87) of the enrolled patients achieved PR after induction therapy, with 10 and 16 patients exhibiting cMRD positivity and negativity, respectively, and the both group achieved similar deep response rate for post-ASCT response (40% vs. 43.7% for VGPR or better) and the best response during the follow-up (60% vs. 66.6% for VGPR or better). Although a clinical significance was found of response post-induction for patients with different cMRD status (52.4% for cMRD+ vs. 76.5% for cMRD-), but the correlation was not found between the cMRD status and the deep response patients achieved during the therapy (P>0.05). And there was no correlation between the depth of pre-ASCT responses and survival (P>0.05). The median follow-up was 26.8 months. The achievement of negative mMRD before ASCT was associated with longer mPFS (P=0.009, 55.88m vs 27.10m) but not mOS (P=0.115, NR vs. 58.86m). Patients with different cMRD status experienced the similar mPFS (P=0.685, 40.54m vs. 76.45m for negativity vs. positivity) and mOS (P=0.885, NR vs. 58.86m for negativity vs. positivity). In patients achieving CR for best response, the presence of MRD negativity predicted longer survival compared with MRD positive CR and VGPR or less in mPFS (P < 0.001, median mPFS, 55.88m vs. 24.74m vs. 27.10m) and mOS (P=0.006, median mOS, NR vs. NR vs. 41.65m).
Conclusions: In conclusion, our results indicate that the SCC contains fewer tumor cells than the BM prior to ASCT, and that the level of cMRD is similar among patients with different responses (PR, VGPR, or CR) before ASCT. Detectable cMRD does not significantly predict the post-ASCT response and survival, highlighting the feasibility of ASCT in patients who have attained PR. In contrast, mMRD status was identified as a significant predictor of a deeper response and longer survival. These results suggest that the post-ASCT response and the best response based on mMRD status during follow-up should be considered valuable indicators of clinical outcomes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal